Before states banned abortion, one of the gravest outcomes of early miscarriage could easily be avoided: Doctors could offer a dilation and curettage procedure, which quickly empties the uterus and allows it to close, protecting against a life-threatening hemorrhage.
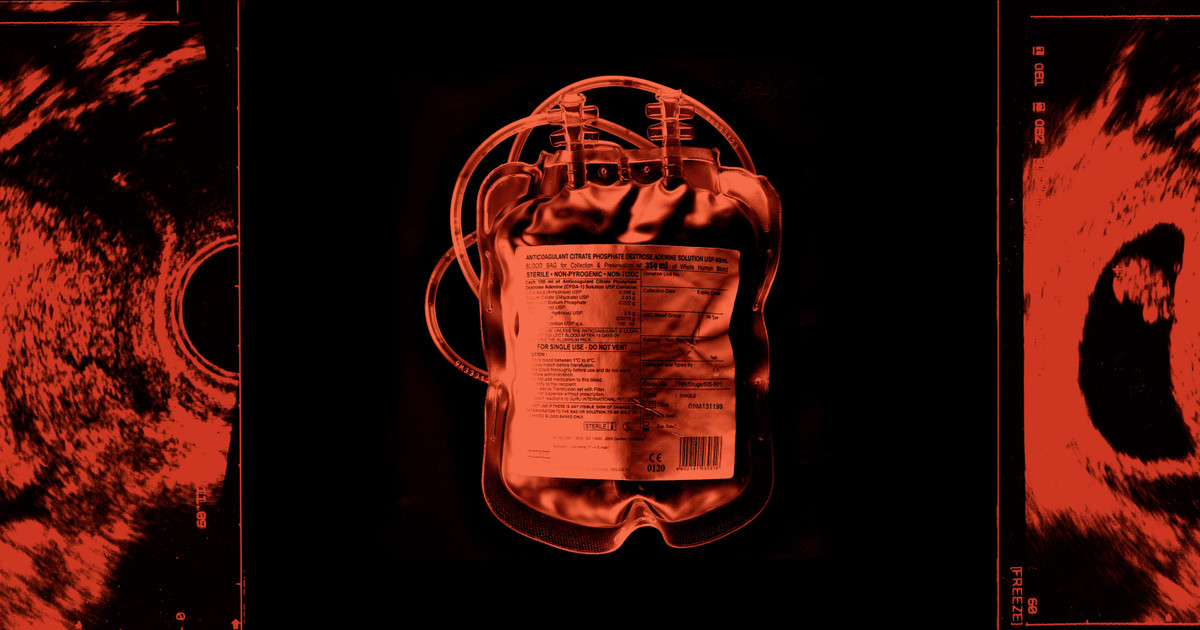
But because the procedures, known as D&Cs, are also used to end pregnancies, they have gotten tangled up in state legislation that restricts abortion. Reports now abound of doctors hesitating to provide them and women who are bleeding heavily being discharged from emergency rooms without care, only to return in such dire condition that they need blood transfusions to survive. As ProPublica reported last year, one woman died of hemorrhage after 10 hours in a Houston hospital that didn’t perform the procedure.
Now, a new ProPublica data analysis adds empirical weight to the mounting evidence that abortion bans have made the common experience of miscarriage — which occurs in up to 30% of pregnancies — far more dangerous. It is based on hospital discharge data from Texas, the largest state to ban abortion, and captures emergency department visits from 2017 to 2023, the most recent year available.
After Texas made performing abortions a felony in August 2022, ProPublica found, the number of blood transfusions during emergency room visits for first-trimester miscarriage shot up by 54%.
The number of emergency room visits for early miscarriage also rose, by 25%, compared with the three years before the COVID-19 pandemic — a sign that women who didn’t receive D&Cs initially may be returning to hospitals in worse condition, more than a dozen experts told ProPublica.
While that phenomenon can’t be confirmed by the discharge data, which tracks visits rather than individuals, doctors and researchers who reviewed ProPublica’s findings say these spikes, along with the stories patients have shared, paint a troubling picture of the harm that results from unnecessary delays in care.
“This is striking,” said Dr. Elliott Main, a hemorrhage expert and former medical director for the California Maternal Quality Care Collaborative. “The trend is very clear.”
The data mirrors a sharp rise in cases of sepsis — a life-threatening reaction to infection — ProPublica previously identified during second-trimester miscarriage in Texas.
Blood loss is expected during early miscarriage, which usually ends without complication. Some cases, however, can turn deadly very quickly. Main said ProPublica’s analysis suggested to him that “physicians are sitting on nonviable pregnancies longer and longer before they’re doing a D&C — until patients are really bleeding.”
That’s what happened to Sarah De Pablos Velez in Austin last summer. As she was miscarrying and bleeding profusely, she said physicians didn’t explain that she had options for care. Sent home from the emergency room without a D&C two times, she ultimately needed blood transfusions so that she wouldn’t die, according to medical records. “What happened to me was just so wrong,” she told ProPublica. “Doctors need to be providing care to pregnant women — that needs to be a baseline.”

Credit:
Ilana Panich-Linsman for ProPublica
After ProPublica exposed preventable deaths following delays in care, the Texas Legislature passed a bill this year to clarify that doctors can provide abortions when a patient is facing a life-threatening emergency, even if it is not imminent.
But many Texas doctors say the reform does not address the difficulty of treating women experiencing early miscarriages, which almost always involve blood loss; they say it’s hard to know when the expected bleeding might evolve into a life-threatening emergency — one that could have been prevented with a D&C. Women can bleed and remain stable for a long time, until they crash.
Texas forbids abortion at all stages of pregnancy — even before there is cardiac activity or a visible embryo. And while the law allows doctors to “remove a dead, unborn child,” it can be difficult to determine what that means during early miscarriage, when an array of factors can signal that a pregnancy is not progressing.
An embryo might fail to develop. Cardiac activity may not emerge when it should. Hormone levels might dip or bleeding might increase. Even if a doctor strongly suspects a miscarriage is underway, it can take weeks to conclusively document that a pregnancy has ended, and all the while, a patient might be losing blood.
Some OB-GYNs and emergency room physicians have long been advising patients to complete their miscarriage at home, especially at Catholic hospitals, even if that is not the standard of care. But now, physicians across the state are faced with a law that threatens up to 99 years in prison, and more are making a new calculus around whether to intervene or even tell patients they are likely miscarrying, said Dr. Anitra Beasley, an OB-GYN in Houston. “What ends up happening is patients have to present multiple times before a diagnosis can be made,” she added, and some of those patients wind up needing blood transfusions.
While they can be lifesaving, transfusions do not stop the bleeding, experts told ProPublica, and they can introduce complications, such as severe allergic reactions, autoimmune disorders or, in rare events, blood cancer. The dangers of hemorrhage are far greater, from organ failure to kidney damage to loss of sensation in the fingers and toes. “There’s a finite amount of blood,” said Dr. Sarah Prager, a professor of obstetrics and gynecology at the University of Washington. “And when it all comes out, you’re dead.”
ProPublica’s findings about the rise in blood transfusions make clear that women who experience early miscarriages in abortion ban states are living in a more dangerous medical climate than many believe, said Amanda Nagle, a doctoral student investigating the same blood transfusion data for a forthcoming paper in the American Journal of Public Health.
“If people are seeking care at an emergency department,” Nagle said, “there are serious health risks to delaying that care.”
Waiting for Certainty
In some clinics and hospitals across Texas, the pressure to definitively diagnose a miscarriage has led to delays in offering D&Cs.
Considering the chance of criminal prosecution, some doctors now default to what many pregnancy loss experts view as an overly cautious method for diagnosing miscarriage: ultrasound images alone, using criteria from the Society of Radiologists in Ultrasound. Relying only on images to diagnose — and discounting other factors, like lab results or clinical symptoms — can take days or even weeks.
Dr. Gabrielle Taper was a resident at a Catholic hospital in Austin when the ban was enacted, and a culture of fear took hold among her colleagues, she told ProPublica. “We started asking, ‘Are we certain that we can document that we’ve met the radiology guidelines?’ as opposed to just treating the patient in front of us,” she said.
If they couldn’t show that the likely miscarriage met the criteria, they often felt they had to discharge patients without offering a D&C. “People are already in distress, and you are giving them confusion, a false sense of hope,” she told ProPublica. “Having to send a patient home knowing they may bleed so much they would need a blood transfusion — when I know there are procedures I could do or medicine I could offer — is just excruciating.”
The hospital where she worked did not respond to ProPublica’s request for comment.
The American College of Obstetricians and Gynecologists does not recommend this approach, advising doctors instead to review the ultrasound as one piece of information among many and counsel patients on all their options.
The Society of Radiologists in Ultrasound said that the guidelines “are not meant to apply in the setting of a life-threatening situation, such as heavy bleeding,” but did not respond to a question about whether it agreed with ACOG that doctors should use a combination of ultrasound images and clinical judgment to assess a pregnancy loss.
Dr. Courtney A. Schreiber, an obstetrics and gynecology professor and expert in early pregnancy care, said that even if a patient wants to let a likely miscarriage complete at home, the medical team should still explain different management options, including medication to speed up the process or a D&C, should symptoms like bleeding get worse.
“It’s our obligation to share information, help manage expectations and keep women safe,” she said.
What happened to Porsha Ngumezi shows how dangerous it can be to delay care, according to more than a dozen doctors who previously reviewed a detailed summary of her case for ProPublica.
When the mother of two showed up bleeding at Houston Methodist Sugar Land in June 2023, at 11 weeks pregnant, her sonogram suggested an “ongoing miscarriage” was “likely,” her doctor noted. She had no previous ultrasounds to compare it with, and the radiologist did not locate an embryo or fetus — which Ngumezi said she thought she had passed in a toilet; her doctors did not make a definitive diagnosis, calling it a pregnancy of “unknown location.” After hours bleeding, passing “clots the size of grapefruit,” according to a nurse’s notes, she received two blood transfusions — a short-term remedy. But she did not get a procedure to empty her uterus, which medical experts agree is the most effective way to stop the bleeding. Hours later, she died of hemorrhage, leaving behind her husband and young sons.
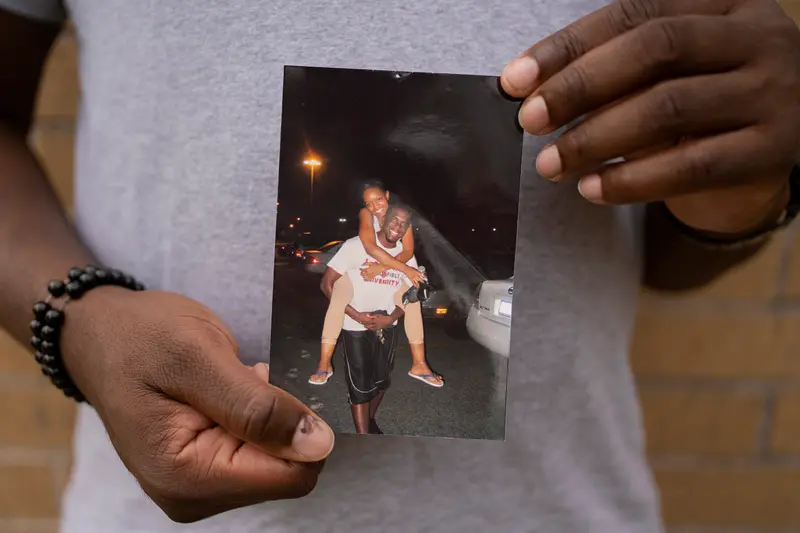
Credit:
Danielle Villasana for ProPublica
Doctors and nurses involved in Ngumezi’s care did not respond to multiple requests for comment for ProPublica’s story last fall, and the hospital did not answer questions about her care when asked about it again for this story. A spokesperson from Methodist Hospital said its OB-GYNs follow ACOG’s miscarriage diagnosis guidelines, which recommend considering clinical factors in addition to ultrasounds.
Visit After Visit
Even in circumstances in which the abortion ban allows a doctor to intervene — to treat a life-threatening emergency, for example, or to “remove a dead, unborn baby” — there’s plenty of evidence, detailed in lawsuits and federal investigations, that doctors in Texas still aren’t offering procedures.
As soon as Sarah De Pablos Velez, a 30-year-old media director, learned she was pregnant last summer, she began attending regular checkups at St. David’s Women’s Care, in Austin. During her third appointment at about nine weeks, a resident, Dr. Carla Vilardo, and her supervisor, Dr. Cynthia Mingea, reviewed the ultrasound, according to medical records, which indicated her pregnancy wasn’t viable. Instead of being offered treatment for a miscarriage, De Pablos Velez says she was advised to hold out hope and come back for the next checkup.
Five maternal health experts and practicing OB-GYNs who reviewed the records for ProPublica said by that ultrasound visit, doctors would have had enough information to determine that the pregnancy wasn’t viable, even under the most conservative guidelines. If they wanted to be extra sure, they could have done blood work or one more ultrasound during that visit.
Instead, De Pablos Velez was told to come back in two weeks, according to medical records. During a visit when she should have been nearly 11 weeks pregnant, Mingea wrote in her chart she was “not optimistic” about the pregnancy’s viability. Still, De Pablos Velez was advised to return in another week to be sure.
Within a few days, when the cramping got so bad she could barely walk, De Pablos Velez went to the emergency room at St. David’s Medical Center, unaware that a D&C could stop the pain and the bleeding. “I’ve never researched what it looks like for women who have a miscarriage,” she told ProPublica. “I always thought you go to the bathroom and have a little bit of blood.”
Over two visits to the emergency room, doctors told her that she could complete the miscarriage at home, even as she reported filling up three toilet bowls with blood and a nurse remarked that they needed a janitor to clean the floor, De Pablos Velez and her husband recalled. No obstetrician ever came to assess her condition, according to medical records, and while her hospital chart says “all management options have been discussed with the patient and her husband,” De Pablos Velez and her husband both told ProPublica no one offered her a D&C.
She was told to follow up with her OB at her next appointment in three days. Six hours after discharge, though, she was trying to ride out the pain at home when her husband heard her muttering “lightheaded” in the bathroom and ran to her in time to catch her as she collapsed. “She was pale as a ghost, sweating, convulsing,” said her husband, Sergio De Pablos Velez. “There was blood on the toilet, the trash can — like a scene out of a horror movie.”
An ambulance rushed her to the hospital, where doctors realized she no longer had enough blood flowing to her organs. She received two blood transfusions. Without them, several doctors who reviewed her records told ProPublica, she would have soon lost her life.

Credit:
Ilana Panich-Linsman for ProPublica
Vilardo and the doctors who saw De Pablos Velez in the emergency room did not respond to requests to speak with ProPublica or declined to be interviewed. St. David’s Medical Center, which is owned by HCA, the largest for-profit hospital chain in America, said it could not discuss her case unless she signed privacy waivers. The hospital did not respond to ProPublica’s questions even after she submitted them. The De Pablos Velezes say that a hospital patient liaison told them after the ordeal that the hospital would conduct an internal investigation, educate the emergency department on best practices and share the results. It never shared anything. When ProPublica asked about the status of the investigation, neither the liaison nor the hospital responded.
Mingea, who supervised Vilardo’s care during checkups, reviewed the clinic’s records with ProPublica and agreed that De Pablos Velez should have been counseled about miscarriage management options at the clinic, weeks before she ended up in the ER. She said she did not know why she wasn’t but pointed ProPublica to the Society of Radiologists in Ultrasound criteria, which is hanging on the clinic’s wall and is used to teach residents.
She was adamant that her clinic, which she described as “very pro-choice — about as much as we can be in Texas,” regularly provides D&Cs for miscarrying patients. “I feel badly that Sarah had this experience, I really do,” she said. “Everybody deserves to be counseled about all their options.”
Doctors had five opportunities to counsel De Pablos Velez about her options and offer her a D&C, said Dr. Jodi Abbott, an associate professor of obstetrics and gynecology at Boston University School of Medicine, who reviewed case records. If they had, the life-or-death risks could have been avoided.
De Pablos Velez “basically received the same care Porsha Ngumezi did, only Porsha died and she survived,” said Abbott. “She was lucky.”
Sophie Chou contributed data reporting, and Mariam Elba contributed research.